When our innate immune system detects a pathogen it mounts a potent inflammatory response that has the capacity to contain and eliminate the infection, but typically also causes significant damage to the inflamed tissue. Acute inflammation is thus followed by an anti-inflammatory tissue-repair response. This critical transition is controlled by a central regulator of inflammation, STAT3.
Some pathogens sabotage the immune system by targeting STAT3 activity to promote premature transition towards the anti-inflammatory response, which allows them to evade inflammatory clearance in the process of establishing chronic infection. Prof. Christoph Dehio’s team at the Biozentrum of the University of Basel has now discovered a new molecular mechanism how bacterial pathogens can activate STAT3 to promote this inflammatory switch.
Bacterial pathogen hijacks host signaling
The researchers initially discovered that the chronically infecting bacterial pathogen Bartonella henselae hijacks host’s signaling pathways and triggers vigorous activation of STAT3. Investigating bacterial proteins injected by a molecular syringe into host cells they then identified the protein BepD as novel activator of STAT3. “We were amazed how robustly BepD was shutting off inflammation,” says Dehio. “This prompted us to work out this molecular mechanism of STAT3 activation.”
BepD forms a signaling hub for STAT3 activation
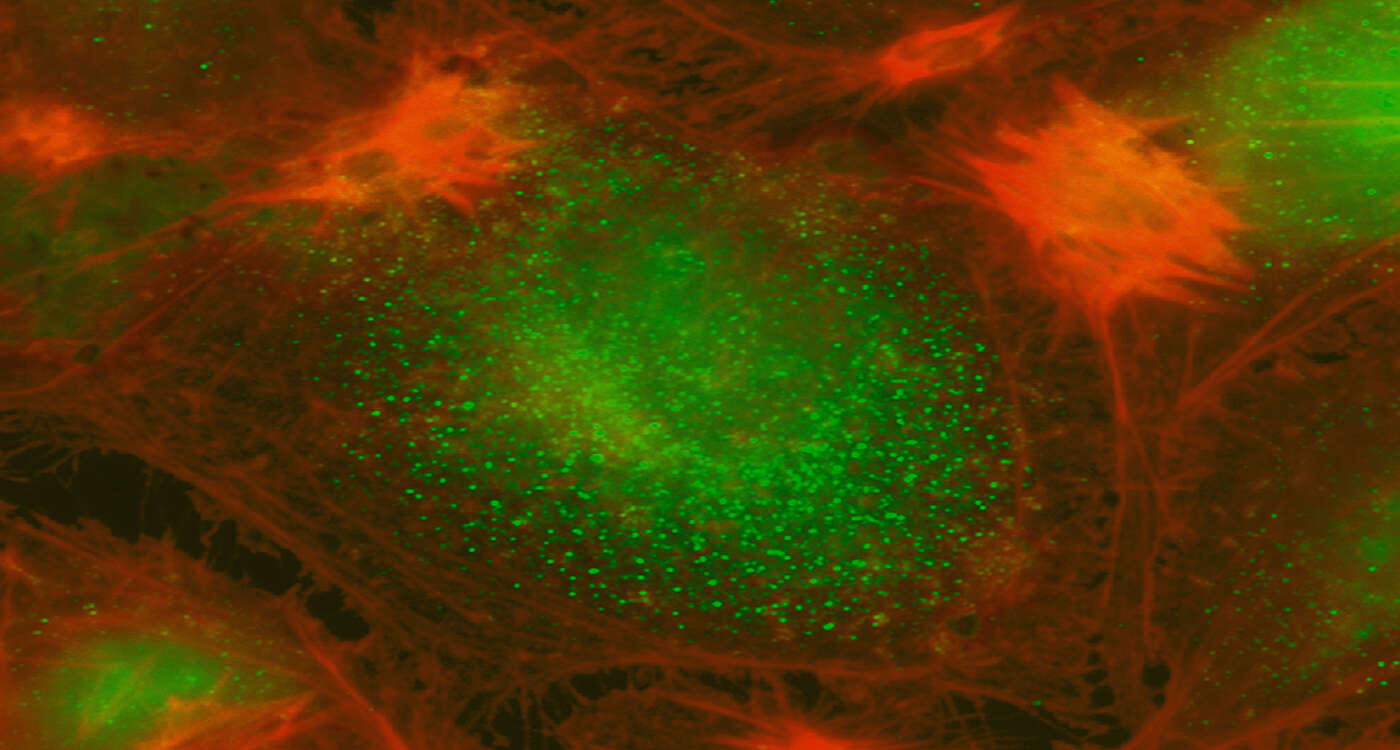
Upon injection into host cells specific units of BepD become chemically modified by host enzymes. These modified units then serve as docking sites for several host proteins, including STAT3 and an enzyme that in turn activates STAT3. “BepD thus serves as a signaling hub for STAT3 activation by recruiting both STAT3 and its activator,” says Isabel Sorg, first author of the study. “Activated STAT3 then forms a dimer and moves to the nucleus where it triggers an anti-inflammatory response program”.
Inspiration for treatment of chronic infections
“In healthy cells STAT3 activity is controlled by extracellular immune modulators via membrane-bound receptors ,” explains Dehio. “In stark contrast, the intrinsic activation of STAT3 by the bacterial protein BepD is independent of any extracellular stimulus.”
Beyond the paradigm of pathogen-induced STAT3 activation and anti-inflammatory response, BepD may also inspire new treatment options for chronic infection and inflammatory diseases.
Original article:
Isabel Sorg, Christoph Schmutz, Yun-Yueh Lu, Katja Fromm, Lena K. Siewert, Alexandra Bögli, Kathrin Strack, Alexander Harms, and Christoph Dehio. A Bartonella effector acts as signaling hub for intrinsic STAT3 activation to trigger anti-inflammatory responses. Cell Host & Microbe; published 11 March 2020.
Contact: Communications