Main Content
Pathogenesis and treatment of chronic bacterial infections
Some bacterial pathogens can persist in the human body for weeks, months, or even years, ultimately causing chronic disease. Understanding how they achieve this long-term survival is essential for developing therapies that can truly eradicate them.
Chronic bacterial infections are a growing global challenge, driven by the rise of antibiotic resistance, an aging population with weaker immune defenses, and the rapid spread of new pathogens through globalization. Many bacteria can evade or disable the immune system, leading to recurrent or relapsing infections that are difficult to treat.
Our research aims to uncover the molecular strategies bacteria use to persist inside the human body and to design treatment approaches that overcome their remarkable resilience to antibiotics and the body’s immune system.
Brucella and brucellosis
Brucella are zoonotic pathogens transmitted to humans through contact with infected livestock or consumption of contaminated animal products. Brucellosis is a chronic, debilitating disease, with relapse rates of 5-15 percent even after prolonged combination antibiotic therapy.
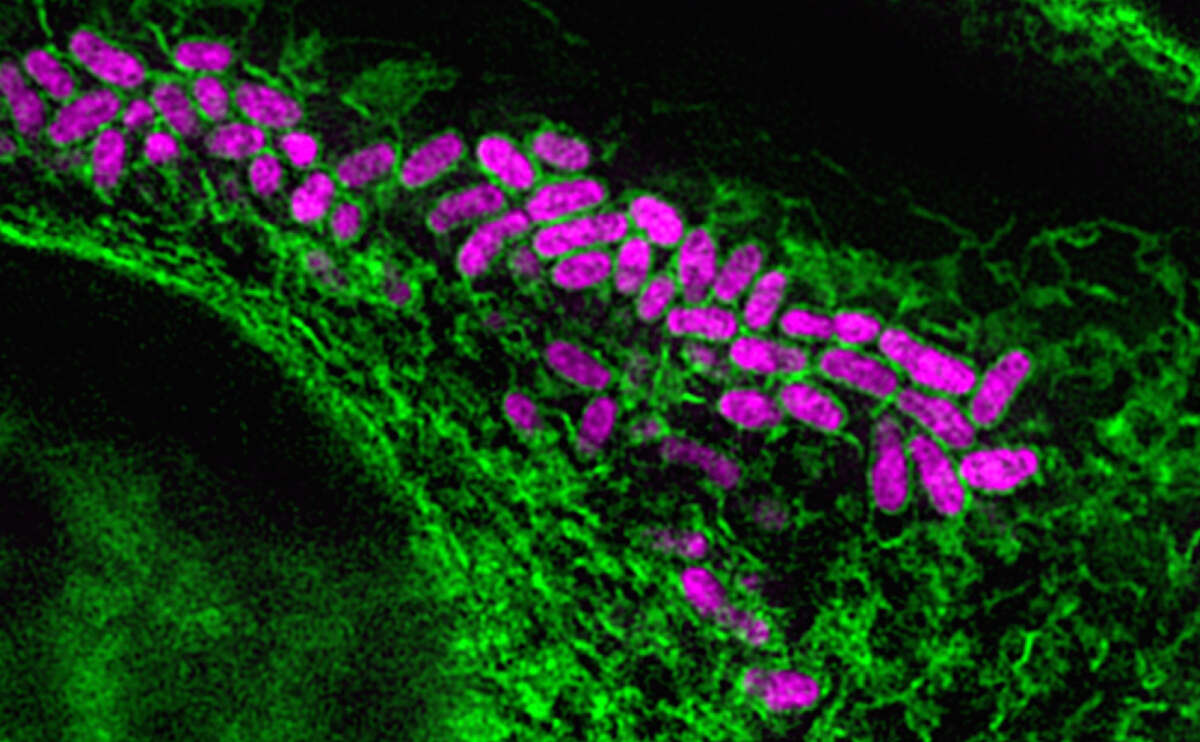
Our lab develops in-vitro infection models that mimic the physiological state of Brucella during human infection. Using these models, we investigate the bacterial and host factors that drive persistence and relapse. A major focus is the type IV secretion system – a specialized molecular machine used by the pathogen to manipulate their host cells to and establish long-term infection. We leverage these models to design and test safer, more effective antibiotic regimens and explore novel therapeutic strategies to break the cycle of chronic brucellosis.
Uropathogenic Escherichia coli and urinary tract infections
Most E. coli strains are harmless and are part of the healthy gut microbiome. However, some strains can cause serious illnesses such as food poisoning, septic shock, meningitis—and urinary tract infections (UTIs). Uropathogenic E. coli (UPEC) is responsible for the majority of UTIs, which are the leading cause of antibiotic prescriptions and a major driver of antimicrobial resistance. Even after standard antibiotic therapy, up to 50 percent of patients suffer recurrent infections, turning an acute problem into a chronic condition.
Our lab creates in-vitro models that replicate the physiological state of UPEC in the human bladder during infection. These models help us identify bacterial and host factors that drive infection, persistence, and recurrence – insights that are critical for developing more effective treatments. We also use these models to test the performance of novel antibacterial agents.